A few cases recently have re-highlighted the lag time in knowledge translation from evidence to clinical practice, so I thought I would use it as an opportunity to summarise some current thinking on myocardial infarction (MI).
When we think about MI, we typically think about STEMI and non-STEMI. We know STEMI patients need urgent revascularisation with thrombolysis, PCI or CAGS, and those with NSTEMI get medical management.
This was how I was taught, and how it seems most are still taught today, but unfortunately it is not ideal.
What we are really interested in is not ECG changes, but whether the patient with a history suggestive of MI has an acute coronary occlusion that is likely to benefit from urgent revascularisation or not.
ST elevation on their ECG is a useful test to predict this, and we have got pretty good at recognising STEMIs, but there are a bunch of other ECG patterns that also predict coronary occlusion.
Some of these we learn about and call STEMI-equivalents, but this still creates a restriction in our thinking around MI, an overfocus on ST elevation (STE), and reduces us to a false dichotomy of STEMI (and equivalents) vs non-STEMI .
The issue with this is not that we are missing MIs, but that we are treating up to 30% of MIs with an acute coronary occlusion as non-STEMIs, without emergent reperfusion therapy and therefore missing an opportunity to give these patients the best possible care and chance of better recovery.
This STEMI/non-STEMI dichotomy has been around for 30 years with little change until recently, when Drs Meyers, Weingart and Smith published the OMI manifesto in 2018.
This proposed a new paradigm of Occlusive Myocardial Infarction (OMI) and, since we need a snappy acronym – NOMI, or Non-Occlusive MI.
Occlusion Myocardial Infarction (OMI) is defined as a branch of the ACS algorithm representing near or total occlusion with insufficient collateral circulation causing active infarction.
Non-Occlusion Myocardial Infarction (NOMI) is defined by no occlusion, or sufficient collateral circulation to avoid active infarction.
Simply put, this divides acute MI (AMI) into those likely to benefit from rapid revascularisation (OMI), and those not likely to (NOMI). Of course this is not perfect either, as one can become the other, and back again, but it is a step in the right direction.
This divide and the patterns to look out for are constantly evolving so we have to keep checking in with the latest updates in this field, but some of the main OMI patterns to be familiar with are listed below.
In the right clinical context the following patterns need urgent reperfusion therapy!
- STEMI
- Women
- 1.5mm STE in V2, V3
or - 1mm STE in any 2 contiguous leads
- 1.5mm STE in V2, V3
- Men
- under 40 years old – 2.5mm STE in V2, V3
- over 40 – 2mm STE in V2, V3
or - All men – 1mm STE in any 2 contiguous leads
- Look for reciprocal ST depression in leads opposite STE
- Pathological Q waves may develop in acute MI (after a few hours) and persist indefinately in 70%
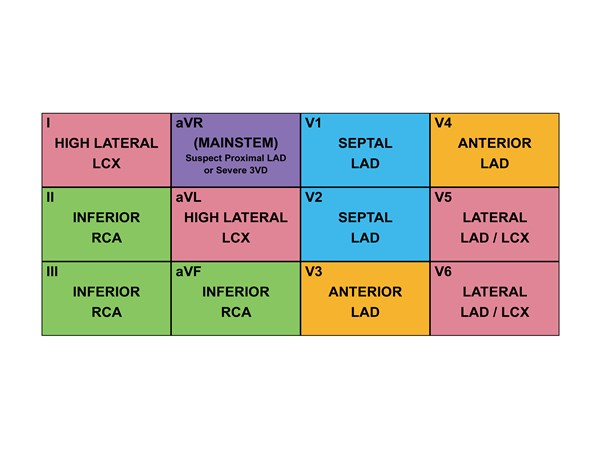
- STEMI subtypes and territories
- Septal
- STE V1-3
- septal artery
- Anterior
- STE V2-4
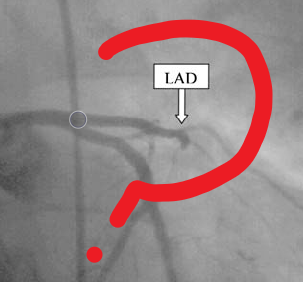
- LAD
- Lateral
- STE I, aVL, V4-6,
- STD inferior
- Circumflex
- Inferior
- STE II, III, aVF,
- STD aVL
- RCA
- Right Ventricle
- STE III>II, V1, V3R-V6R
- (STD V2)
- RCA
- Posterior
- STE V7-9 (0.5mm)
- RCA >> LCA
- All these patterns may overlap and merge depending on the vessels occluded
- Women
- Posterior STEMI
- Horizontal ST depression in V1-3
- Dominant R wave V2 (=reciprocal posterior Qwave)
- Upright T waves
- These ECG changes are the reciprocal of the posterior STE
- (STE V7-9 as above)

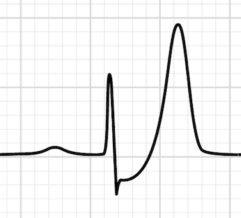
- Hyperacute T waves
- No agreed definition
- Broad symmetrical prominant T waves
- Especially in context of STE/reciprocal changes
- Part of continuum of ECG change in STEMI i.e. will progress to STE
- May normalise if spontaneous reperfusion
- Rule out hyperkalaemia
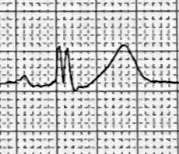
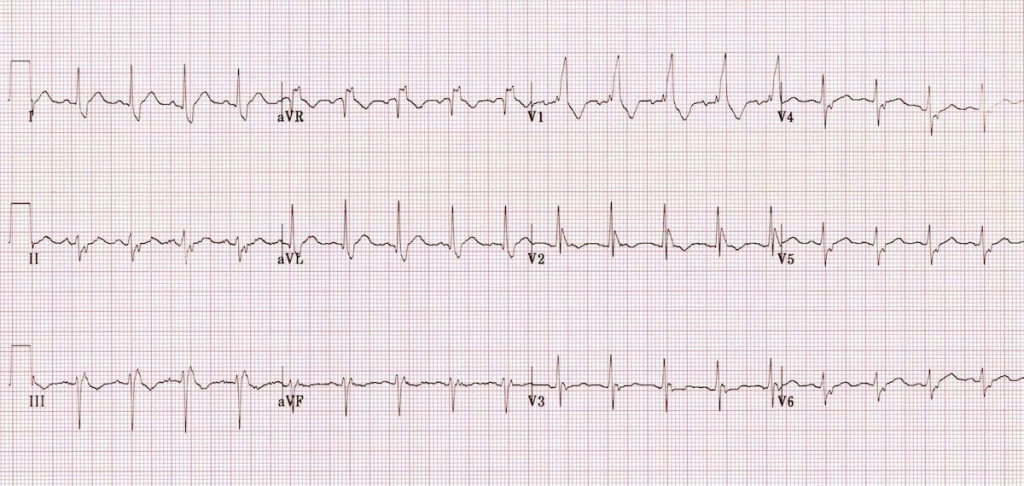
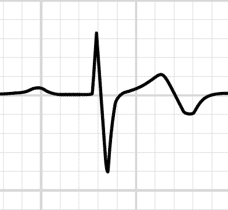
- De Winter’s T waves
- Large peaked T waves in precordial leads with upsloping ST depression
- +/- 0.5-1mm STE in aVR
- May be followed or preceded by classic STEMI pattern
- Represent 2% of cases of LAD occlusion
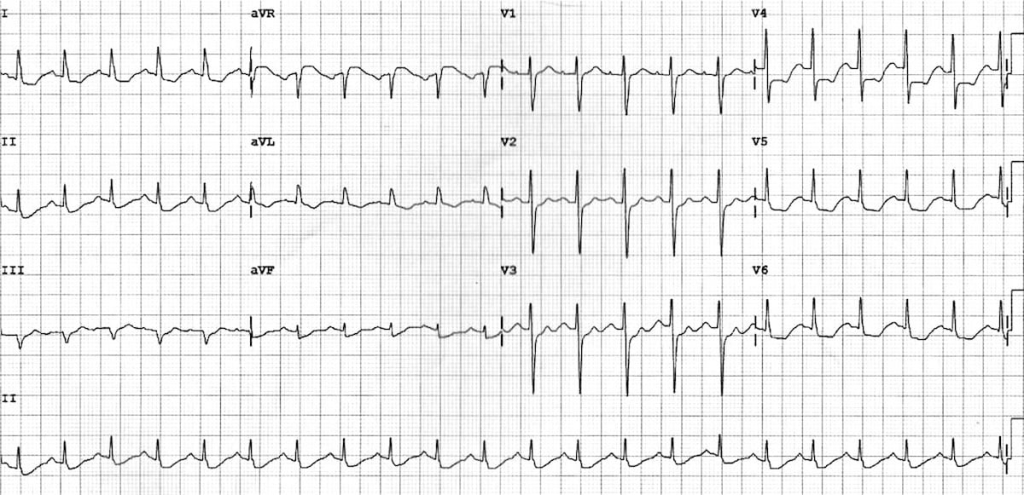
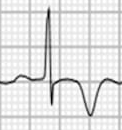
- Wellen’s Syndrome
- Biphasic (type A) or deeply inverted (type B) T waves in V2-3
- Highly specific for critical LAD stenosis
- Patient often painfree (changes are identical to reperfusion ECG changes)
- LAD may reocclude with hyperacute T waves and STEMI
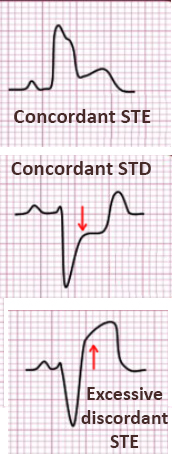
- LBBB with Smith-Modified Sgarbossa Criteria
- New LBBB by itself is no longer a criterion for urgent revascularisation unless the patient is haemodynamically unwell.
- Positive on any of Sgarbossa Criteria = 98% probability of OMI
- Concordant STE ≥ 1mm in ≥ 1 lead
- Concordant STD ≥ 1mm in ≥ 1 lead of V1-3
- Proportionally excessive discordant STE in ≥ 1 lead anywhere with ≥ 1 mm STE, defined by ≥ 25% of the depth of preceding S-wave
- New bifasicular block
- In the context of cardiac chest pain, RBBB + LAFB are highly associated with proximal LAD occlusion
- Look for subtle ST changes
- Shark Fin morphology
- Extreme J-point and ST elevation merging with QRS
- Sign of acute coronary occlusion requiring reperfusion
- Easily mistaken for hyperkalaemia or VT
- Acute ischaemia in LVH
- STE ≥ 25% QRS
and - STE in ≥ 3 contiguous leads
or - T inversion V1-3
- STE ≥ 25% QRS
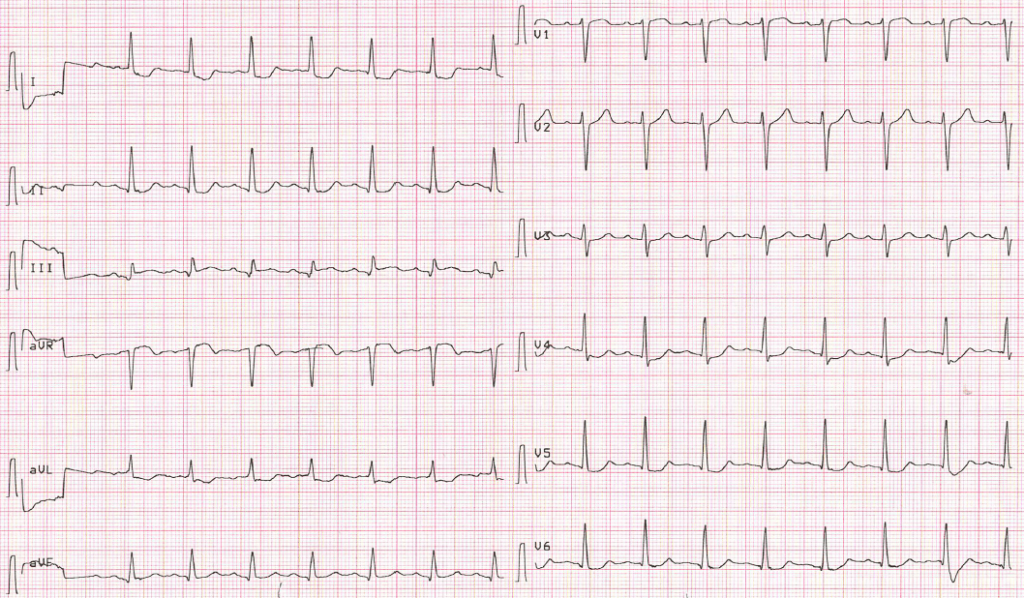
- STE in aVR and/or widespread ST depression
- ≥ 1mm STE in aVR = LMCA > LAD
- This pattern is concerning for high grade left main coronary artery (LMCA) or LAD stenosis, (or complete occlusion with collateral circulation)
- It is a non-specific sign of global cardiac ischaemia (so can be seen in other conditions causing this)
- Complete occlusion leads to cardiogenic shock and death
- It is an indication for urgent but not necessarily immediate PCI
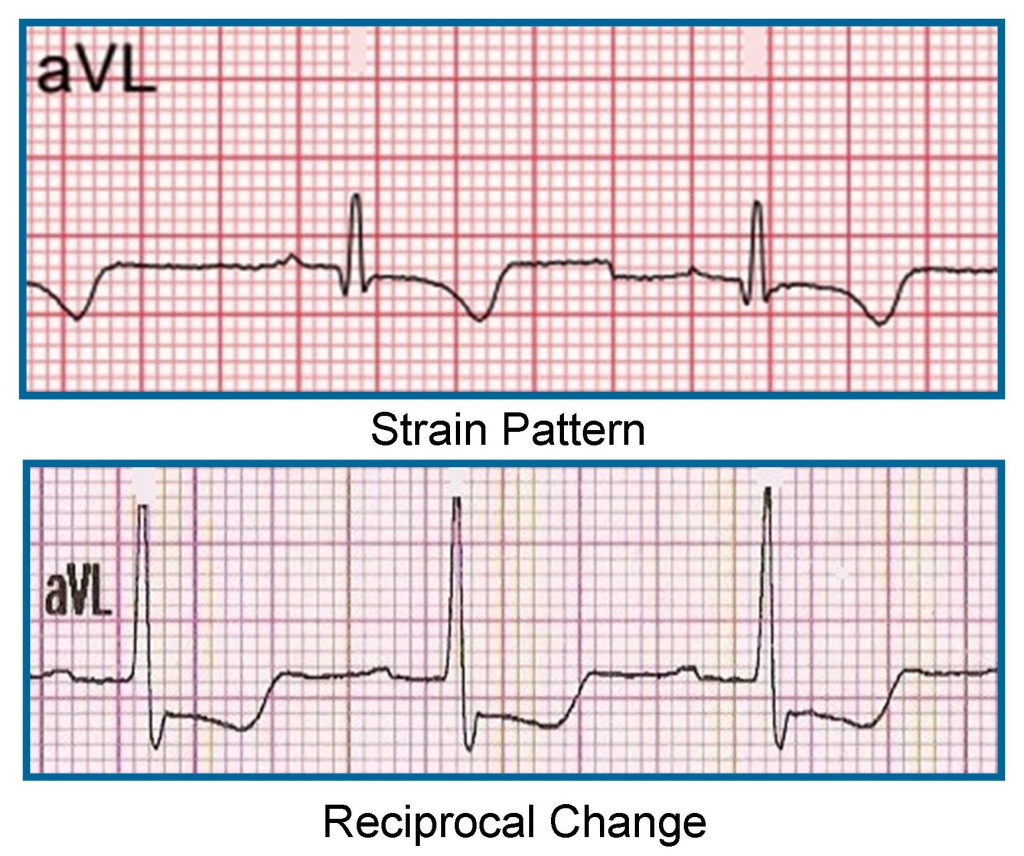
- T wave inversion in aVL
- Symmetrical T wave inversion +/- STD in aVL is specific but not sensitive for mid-LAD occlusion
- It can also be seen in evolving inferior MI with possible RV involvement
- Commonest reason for aVL T inversion is strain in setting of LVH
- Aslanger pattern
- Inferior STE in lead III only
- Concomitant STD in any of V4-V6, with a positive/terminally positive T-wave
- ST segment in V1 > V2
- Associated with inferior OMI
I’m sure these patterns will come and go as new evidence emerges. Ultimately, if the ECG looks funny (even in the absence of STEMI criteria) or the patient is unwell or has ongoing ischaemic pain, consider whether it could be an occlusive MI requiring reperfusion.
There is much more to read on this topic, so I’ve attached a list of resources below.
Feel free to comment if you have any thoughts or experiences to share.
- This is the paper proposing coronary occlusion as the cause of MI
- Replacing the STEMI misnomer
- The DIFOCCULT trial
- The OMI manifesto
- The history of coronary perfusion
- The history of thrombolysis
- AU/NZ Cardiac Guidelines
- LBBB with MI
- STEMI equivalents
- ST elevation in aVR
- Dr Smith’s ECG blog in general
- Shark Fin
- aVL changes
- LVH vs STEMI
- Aslanger Pattern OMI
Cheers,
James