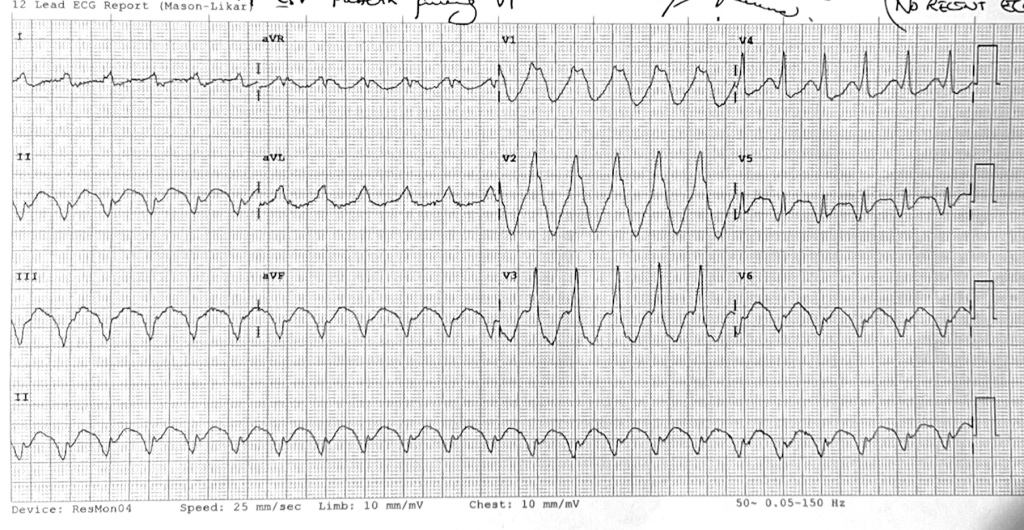
Assuming you don’t have eye floaters and are seeing the same squiggly lines as me, let’s try and figure out what we are looking at.
This is the ECG of a 90 year old man who is conscious but with palpitations and low blood pressure.
Assess and interpret the ECG, think about what the differentials are and how are we going to treat this guy, then click below to work through the answer.
Click here for answers
- Wide complex tachycardia
- Regular
- Rate ~150bpm
- Normal conduction intervals
- Normal QRS
- No hypertrophy
- 2mm ST elevation in V2 and V3, no reciprocal changes
- Pronounced ?hyperacute T waves V2 and V3
So what are the differentials?
For a broad complex tachycardia, we need to consider the following:
- Ventricular Tachycardia
- Supraventricular Tachycardia with abberent conduction
The main causes of abberent conduction include:
- Bundle branch block (left or right)
- Pre-excitation (Wolff-Parkinson White Syndrome)
- Sodium channel blockade (e.g. tricyclic or local anaesthetic toxicity)
- Ventricular pacing (unlikely to be associated with tachycardia)
- Hyperkalaemia (unlikely to be associated with tachycardia)
- Hypothermia (unlikely to be associated with tachycardia)
Obviously the history and examination will give us some clues about the above possibilities, but how do we differentiate VT and SVT with aberrency on the ECG?
There are various criteria which I will link to, but the main factors which make it more likely to be VT include:
- AV dissociation
- Fusion and/or capture beats
- Absence of typical LBBB or RBBB morphology
- Positive or negative concordance in V1-6
- Extreme (north-west) axis
- QRS >160ms (4 small squares)
- Age >35
- Cardiac history or family history of sudden cardiac death
- Of course patient history and old ECGs are also invaluable
In this case:
- There is no obvious AV dissociation (no p-waves)
- No fusion or capture beats
- There is atypical RBBB morphology with R>R’ in V1
- Left axis deviation
- QRS <160ms
- This patient is elderly with a cardiac history
On balance, this ECG is most likely to represent conscious VT. The treatment options are medical management vs DC cardioversion.
Whether VT or SVT, if the patient is haemodynamically unstable treat as unstable VT with urgent DC cardioversion.
This patient was successfully cardioverted and his symptoms improved.
For more detail and examples of VT vs SVT click here and feel free to comment below.
Cheers!
James

2 responses to “What are these squiggly lines I see?”
It is a good explanation about VT . If someone with VT morphology, esp elderly can it be treated as VT regardless cos chance of VT is more than. 90% to SVT with aberrancy. . Can Josephine sign and brugada sign be applied to differentiate between VT and SVT with aberrancy? I like the explanation about the causes. Thank you!
LikeLike
Consider the Brugada Criteria for distinguishing VT and SVT with aberrancy, but most importantly play it safe and treat as VT if uncertain or the patient is unwell.
LikeLike